Statement of Jocelyn Frye, President of the National Partnership for Women & Families WASHINGTON, D.C. – April 17, 2024 – The National Partnership for Women & Families today announced the addition of Jennifer M. Ng'andu to the Board of Directors and...
Childbirth Connection
With so much information out there on pregnancy and childbirth, it’s hard to know what to trust. But it’s important to become informed, because the care you receive during this time can have a big impact on your health, your baby’s health and your overall satisfaction.
To make informed decisions, women need access to evidence-based information and help navigating their maternity care throughout their pregnancy and birth journey. That’s why, for nearly 100 years, Childbirth Connection (now a core program of the National Partnership for Women & Families) has connected women with just that kind of high-quality information.
We hope this information will empower you to take charge of your maternity care and guide you in making the best possible decisions for yourself and your baby.

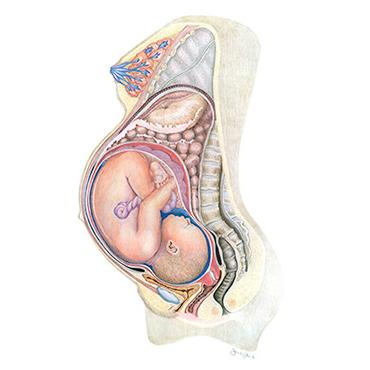
Your Body throughout Pregnancy
Wondering about all the amazing (and sometimes weird) changes taking place in your body during pregnancy?
Check out this slideshow on the effects of pregnancy on your body and the stages of fetal development. The image here illustrates a pregnancy at 40 weeks, or full term.
Listening to Mothers in California
The National Partnership for Women & Families released a new report that reveals the disconnect between the care women seek and the care they receive.
Listening to Mothers in California explores the views and experiences of childbearing women with an in-depth focus on maternity care.


